Co-infection with multiple pathogens presents a significant challenge to global health, particularly in regions with high disease burden and limited healthcare resources. Among the most prevalent co-infections are those involving HIV-1, tuberculosis (TB), malaria, and hepatitis C virus (HCV).
In this blog, we'll explore the interplay between these infectious diseases, their impact on health outcomes, challenges in diagnosis and treatment, and strategies for effective management.
HIV-1 and Tuberculosis
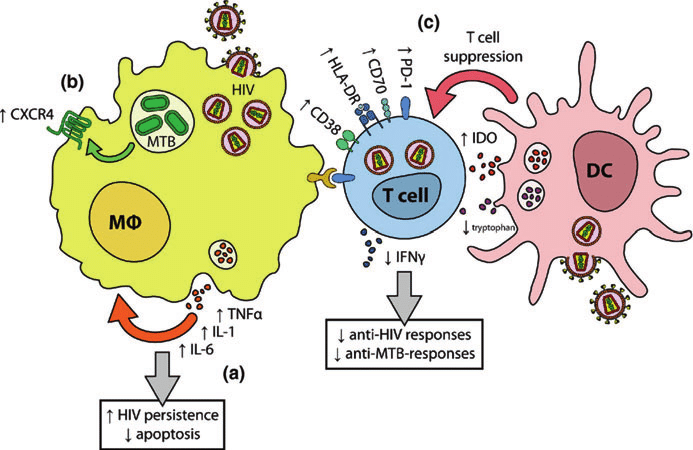
HIV weakens the immune system, making individuals more susceptible to opportunistic infections like tuberculosis. TB is one of the leading causes of death among people living with HIV. Co-infected individuals face complex challenges in diagnosis and treatment, as TB symptoms may be masked by HIV-related symptoms, leading to delayed diagnosis and increased transmission risk. Additionally, drug interactions between antiretroviral therapy (ART) and TB medications can complicate treatment regimens
Malaria and HIV-1
Malaria and HIV-1 often coexist in regions where both diseases are endemic. Co-infection can exacerbate the severity of both diseases and increase the risk of complications. HIV-1 compromises the immune response to malaria, leading to higher parasite levels and more severe symptoms. Conversely, malaria can accelerate the progression of HIV by increasing viral replication and decreasing CD4 cell counts
Hepatitis C Virus and HIV-1
Co-infection with HIV-1 and hepatitis C virus (HCV) is common, particularly among people who inject drugs. Both viruses share similar routes of transmission, leading to high rates of co-infection. Co-infected individuals experience faster progression of liver disease, higher rates of liver-related complications, and reduced response to HCV treatment compared to those infected with HCV alone.
Managing co-infection requires specialized care, including close monitoring of liver function, drug interactions, and adherence to treatment
Challenges and Strategies
Diagnosing and managing co-infections pose significant challenges due to overlapping symptoms, limited access to diagnostic tools, and resource constraints in affected regions.
Integrated approaches to healthcare delivery that address multiple diseases simultaneously are essential for improving outcomes.
This includes strengthening healthcare systems, expanding access to diagnostic testing and treatment, and implementing preventive measures such as vaccination and vector control
--> Co-infection with HIV-1, tuberculosis, malaria, and hepatitis C virus presents a formidable challenge to global health.
Addressing these complex interactions requires a multifaceted approach that encompasses prevention, diagnosis, and treatment strategies tailored to the needs of co-infected individuals. By working collaboratively across disciplines and sectors, we can reduce the burden of co-infections and improve the health and well-being of affected populations worldwide.